This month we published the first ever fMRI brain imaging study of health care rationing decision making
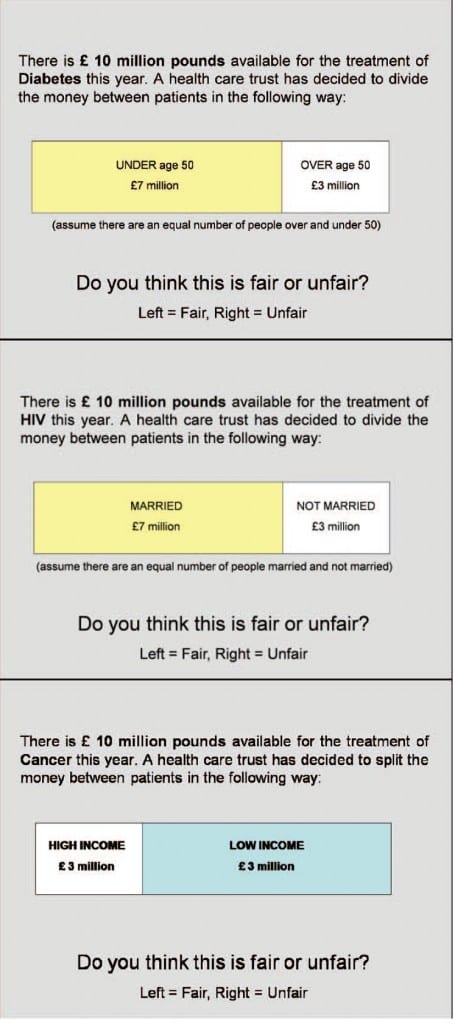
Health care funders around the world have to make difficult moral decisions to allocate limited money to treat various medical conditions in different groups of patients. For example whether or not to support funding for expensive new drug treatments for a group of cancer patients with low chance of survival relative to a drug that will benefit a group with a higher chance of survival. A commonly used framework on which these decisions can be based are Quality Adjusted Life Years or “QALYs”. This system is based on so-called utilitarian decision making principles, which prioritize choices that deliver the maximum benefit to the greatest number of people. The problem with QALYs is that decisions based on this approach are often viewed negatively by members of the general public. People instead believe that everybody has a “right” to receive medical care and anything that violates this principle is unfair and immoral.
Consistent with previous work, when asked to judge the “fairness” of various scenarios depicting a split between different social groups our participants judged unequal division of funding as “unfair”, even when principles of QALY might indicate otherwise. Interestingly brain regions linked to emotion as well as cognitive processes were active during decision making. Unequal splits of resources for medical care produced activity in the anterior insula, a region often associated with social / moral disgust (see earlier posts on social norms and eating disorders). Further, under conditions where participants were prepared to judge unequal splits as fair, more activity was seen in the inferior frontal cortex, a region activated when humans inhibit a strong response impulse.
The results represent a preliminary first step for cognitive neuroscience into the field of health economics and the paper is careful to avoid over interpreting the findings and applying them to real situations outside the scanner. But the findings are consistent with a bigger idea that humans have two decision making systems, one cognitive and one more emotional / instinctive. Given enough information people may be more inclined to support healthcare decisions based on QALYs, but this requires cognitive effort to over-ride a more emotion based bias towards absolute equality and universal rights.
The paper is out i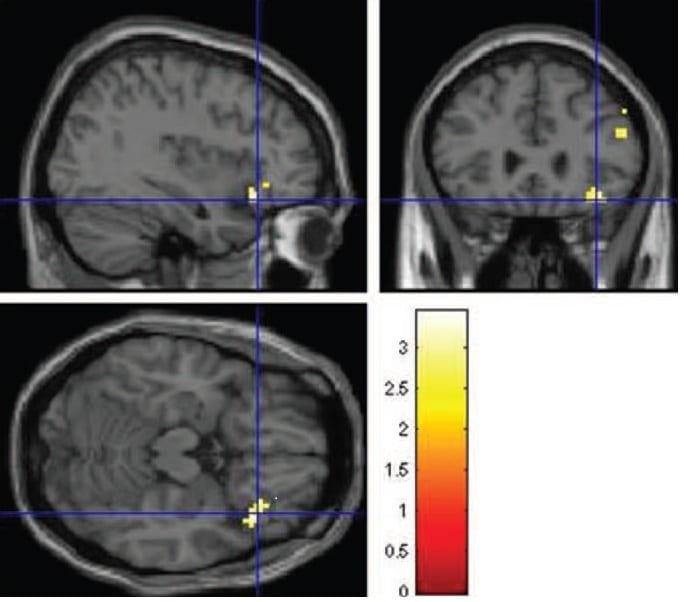 n the June edition of the Journal of Neuroscience Psychology and Economics. The research was carried out in collaboration with Prof. Paul Anand ( Open University and Health Economics Research Centre at the University of Oxford), Lisa Smith (Flinders University Austrailia) and the Exeter Magnetic Resonance Research Centre. A pre-print of the paper is available via the Lincoln Repository website.
n the June edition of the Journal of Neuroscience Psychology and Economics. The research was carried out in collaboration with Prof. Paul Anand ( Open University and Health Economics Research Centre at the University of Oxford), Lisa Smith (Flinders University Austrailia) and the Exeter Magnetic Resonance Research Centre. A pre-print of the paper is available via the Lincoln Repository website.