This month we published a paper in the International Journal of Language and Communication Disorders entitled “Gaze-speech coordination during social interaction in Parkinson’s disease“. The research used mobile eye tracking to examine how people with and without Parkinsons use eye movements during spoken conversation. In order to get people talking we asked them to play a card guessing game, based on the children’s guessing game “HedBanz” in which one player has to describe an object written on a card and the other player has to guess. A link to the full open access publication is available here.
Previous research has shown that eye movements are important in signalling “turn taking” in conversation, whereby the speaker indicates to their conversation partner that the end of the speech turn is coming. Although you might not be aware that you are doing it, we often direct our eye gaze towards the other persons face to indicate it is their turn to speak next. Other work by myself and others has shown how the voluntary control of eye movements is affected in Parkinsons disease. Taking these findings together, we wondered if there were differences in how patients used their eyes during speech and conversation.
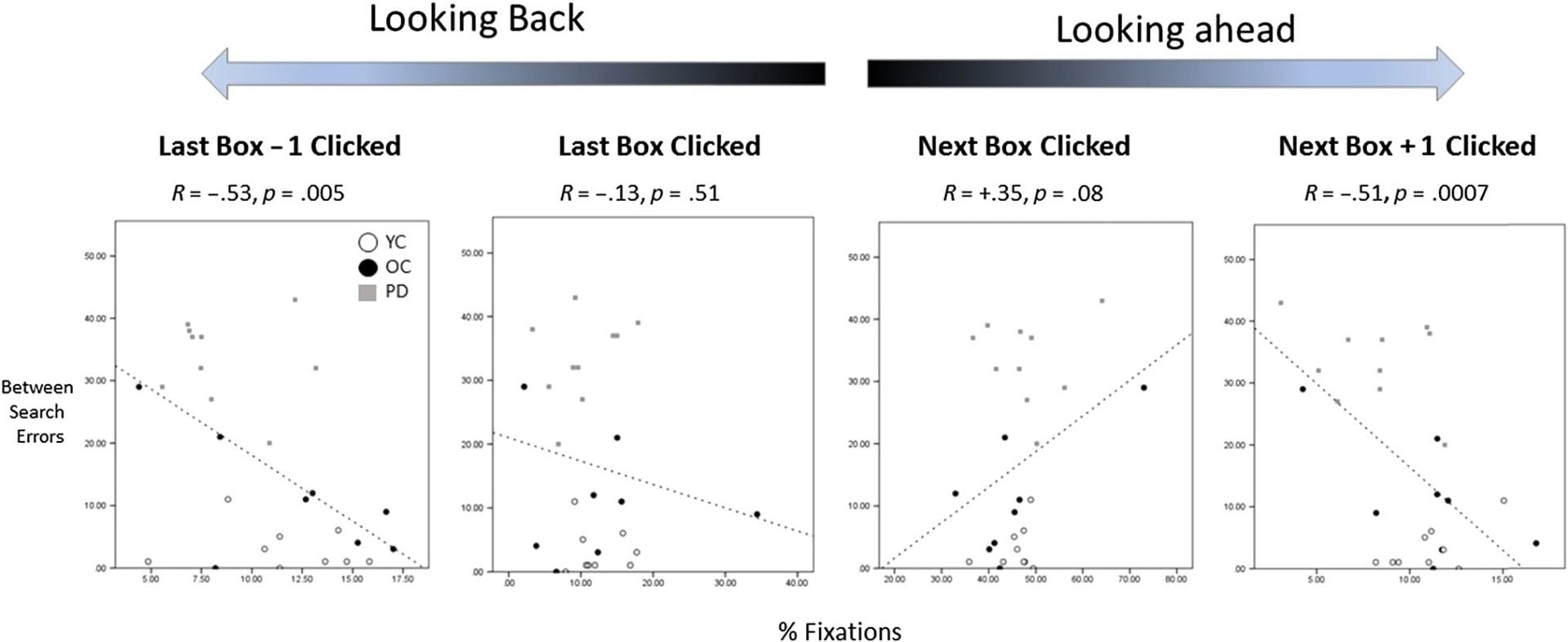
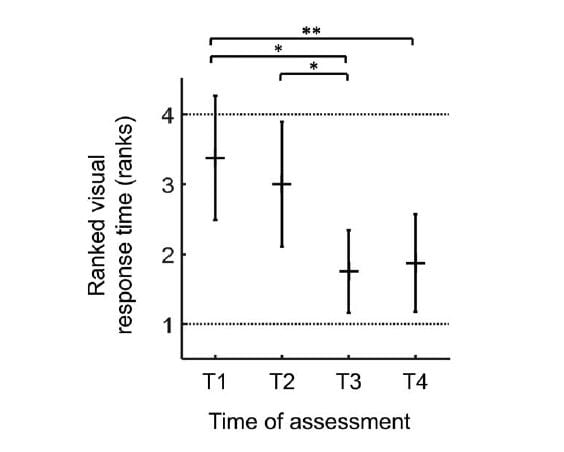
The results showed that people with Parkinsons tend to make longer duration periods of eye fixation on the other persons face and elsewhere. They did less well when describing cards to the other player, suggesting problems with speech, but guessed just as many objects when listening to someone else describing, suggesting that their condition didn’t affect their ability to understand others. We also found that the timing of speech turns was subtly different when a patient was playing the game, with a tendency towards shorter gaps and more interruptions in speech, indicating people with Parkinsons may be slightly more impulsive and sometimes “jump in” to interrupt others more.
The results confirm something I have personally noticed about people with Parkinsons over the years: That they sometimes have a subtly different pattern of gaze during conversation including extended periods of eye contact. This can be slightly disconcerting if you are not aware of it and together with phenomena like reduced facial expression might adversely affect social interaction and communication. We think that wider public knowledge and awareness of some of these more subtle features of the condition could itself improve the quality of life and social connectedness of people with Parkinsons.
The research was conducted in collaboration with Gemma Ezard (Lincolnshire NHS) and Frouke Hermans (formerly University of Lincoln now at the Open University in the Netherlands) and was funded by BA/Leverhulme small grant Ref: SG152231